L4 lumbar spine reflex

L4 lumbar spine reflex pertains to the medial hamstring tendon. There's a potential confusion here; we are talking about the vertebra, and even that's not clear.
Most commonly when the L4 vertebra subluxates it affects the fifth lumbar nerve root; that's clear as mud, you probably think, but it's the way it is.
We could equally have called this page the L5 lumbar nerve root reflex.
Or even the L5 medial hamstring reflex would perhaps have been even better.
When I was in school, back in the last millennium, we were taught the deep tendon reflexes for the leg could only be tested for the L4 and S1 nerve roots. There was none for L5.
It was a canny chiropractor, Dr Lee Arnold, who taught me how to test for L5; by tapping on the tendon of the medial hamstring. Notice in the graphic above how it's barely visible on the left, whilst the right is very prominent.
This is important as it is used to confirm a disk herniation, usually between L4/L5, but it can be lower; more about that later.
Pressing on the medial hamstring tendon on the right it has a very firm, taut feel about it; but that on the left is quite different; the patient has a severe L4/L5 disc herniation.
Along with this condition, there will usually be loss of great toe extension; you can't easily lift it off the ground.
Both Lasegue's straight leg raise and the Slump test for sciatica will be strongly positive; in particularly nasty cases like this one, the crossed sign is evident; raising the opposite lower limb reproduces the pain in the involved thigh or calf.
L4 lumbar spine reflex
There are three ways to test the L4 lumbar spine reflex; that of the L5 nerve root, remember.
L4 lumbar spine reflex goes along with severe lower leg pain and inability to raise the big toe.
Test 1
With the patient lying in the prone position, place your thumb on the tendon, first noting the tension by palpation, and then tap directly on the distal digit, watching to see if it elicits a contraction of the medial hamstring.
As always compare with the opposite limb.
Test 2
With the patient lying supine, the knee almost straight, externally rotate the lower limb and place the index finger over the medial hamstring tendon.
Again feel for the normal tension in the tendon, or absence thereof.
Tap on the index finger, watching for a contraction of the medial hamstring.
Test 3
Less ideal, since the knee is bent and the tendon of the medial hamstring is under less tension, the L4 lumbar spine reflex, L5 nerve root, can be tested sitting; this is convenient as the Patella and and Achilles reflex are often tested thus.
Place the index finger on the medial hamstring tendon, tapping directly and feeling for the jerk; it's more difficult to visualise the contraction of the muscle.
If on Test 3 I am uncertain of a normal reflex, I would normally repeat it, using the first or second procedures.
In the most severe cases of a sciatica, with a prolapse into the intervertebral foramen, the pain in the leg is immediately reproduced by extension and lateral flexion to the same side; the nerve root is caught in a pincer action between the facets.
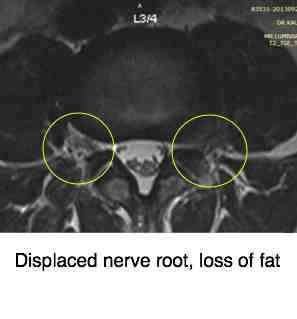
A cardinal sign on the axial view of the MRI is loss of the white fatty deposit in the foramen; it's squished out by the herniated disc, forcing the nerve root between the facets.
You can see more at femoral nerve damage link below.
The last common feature of a patient with a herniated L4/L5 disc, is an inability to raise the big toe as seen below. Or there may be partial weakness; if the examiner presses down on the toe, against resistance, paresis may be detected.
The tendon of the muscle that has become weak is shown.

Every case where there is loss of the L4 lumbar vertebra reflex, the L5 nerve root, and an inability to extend the great toe, together with strongly resisted sciatic stretch tests causing pain in the leg, is a great challenge at the chiropractic coalface.
Interestingly the muscle strength returns, the pain and disability resolve, but very often the L4 lumbar spine reflex does not return; it is not of great consequence.
If the crossed sign is also present, then in my book the patient must take several weeks off work following to the letter our slipped disc rules.
Continuing to travel to work and sitting all day, or labouring, will mean that the case is lost before even getting started; surgery is imminent.
For the patient who resolutely wants to avoid the risks associated with surgery, and is willing to work his or her chiropractor, a successful resolution of the prolapsed disc is possible, even when there is loss of the L4 lumbar vertebra reflex; remember the L5 nerve root.
Bed rest alone is useless, but combined with gentle lower back exercises every half an hour, ice pack compresses and chiropractic adjustments, regularly for at least a month, with occasional follow up thereafter, there is every chance of success.
Having personally suffered from a prolapse into the foramen, with a sequestered fragment directly into the spinal canal, and treated many such cases, I can vouch for the fact that chiropractic can manage these cases; but every one is a challenge, setbacks are common and a gritty determination is demanded of both patient and chiropractor to avoid surgery.
In my own case, it required 18 chiropractic adjustments over a period of five weeks, daily initially; the pain in the leg was much reduced within two weeks, but it was three months before I could confidently do heavy work in the garden, lift a beehive, or even sit for a prolonged length of time; some tingling and numbness in the leg return occasionally, but the pain, muscle weakness and disability have resolved completely.
Research
Incidentally, in cases of L5 radiculopathy, where what I have called the L4 lumbar spine reflex, since that is the vertebra that is most commonly adjusted in the successful resolution of these cases with chiropractic, it is not only my opinion that this is a valid and necessary part of the neurological work up of the patient with a severe sciatica.
In research reported in Surgical Neurology International, entitled "diagnostic performance of the medial hamstring reflex in L5 radiculopathy" the authors demonstrate that this reflex is even more reproducible than the Achilles reflex for a S1 sciatica.
Did you find this page useful? Then perhaps forward it to a suffering friend. Better still, Tweet or Face Book it.
