Spondylolysthesis case file
Spondylolysthesis case file comes about after years of heavy wear and tear in the lower back making it weak and unstable.
If you are a layperson, do not worry, we will explain exactly what a spondylolysthesis case file is all about.
It surely is a jaw-breaker, so we call it a spondy. There are two kinds.
1. Pars inter-articularis fracture
The term "spondylo-lys-thesis" is normally associated with a childhood fracture in the lumbar spine, through a narrow isthmus of cartilage that has not yet turned to bone. Invariably it goes undetected in the small child.
This fracture is called a "spondylo-lysis". It occurs through the so-called "pars inter-articularis", that narrow isthmus of bone that lies between (inter) the two articulating facets, one superior, and the other inferior.
Each vertebra has two inferior facets that articulate with the two superior facets of the vertebra below it. Notice the locking mechanism: the inferior facet of the vertebra above locks onto the superior facet of the vertebra below preventing any possibility of a forward slip. Unless...
The fracture may occur only on one side (unilateral) in which case it usually does not have great clinical significance. However, if it occurs on both sides, then the body of the vertebra is free to slide forwards: a "spondy" in jargon.
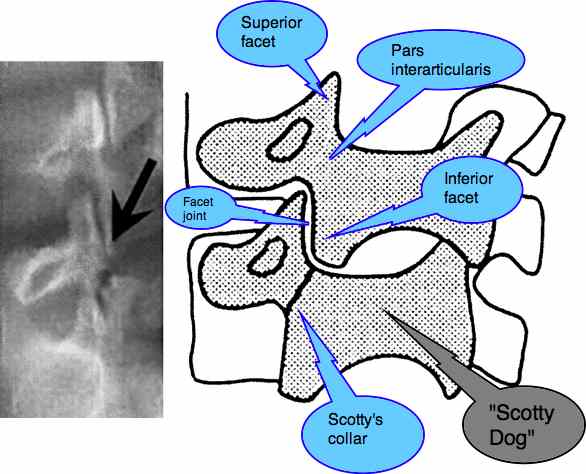
Does Scotty have a collar?
On an oblique X-ray, the clinician is always asking the question, "Does Scotty have a collar?" Can you visualise the Scotty Dog? Between his ear (the superior facet) and his front leg (the inferior facet) lies the narrow isthmus of bone that is prone to fracture in the young child. This is known as "spondylolysis".
Generally, a stable spondylolysthesis due to fracture through the pars causes a gnawing ache, but no great dramas. They certainly can be difficult, especially if associated with further trauma later in life.
Worse is the second type, which is what this case file is about. The degenerative spondy, encountered in the older person, and quite unrelated to the Type I pars fracture type, is rarely stable.
2. Degenerative facet spondy
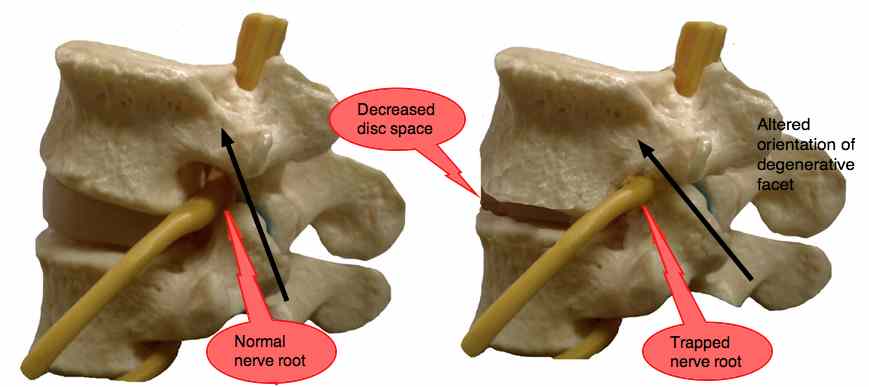
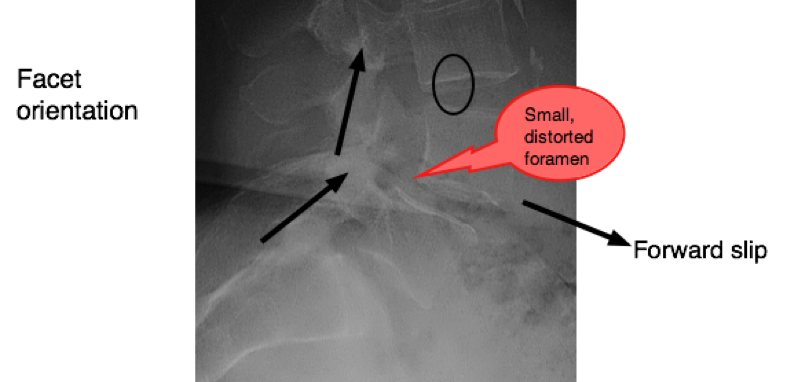
Two things to notice in the diagram:
- The size of the foramen where the nerve emerges is determined by the disc height. As there is loss of disc space, so the foramen becomes smaller, top to bottom.
- As the orientation of the facets becomes more horizontal, see the arrows above, due to degeration of the hyaline cartilage, the vertebra is able to slide forward (spondylolysthesis), distorting and further decreasing the size of the foramen.
HYALINE CARTILAGE ... what makes it degenerate?
Spondylolysthesis case file (type 2)
Spondylolysthesis case file explains the pain behind this syndrome; this is the wear and tear kind.
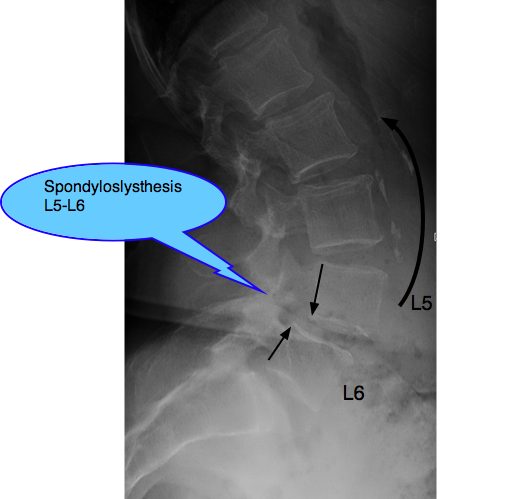
X-RAY REPORT @ SPONDYLOLYSTHESIS CaseFile
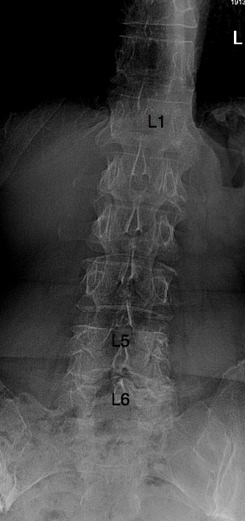
There are six lumbar vertebrae (normally five). The body of L5 has moved anterior on L6, owing to degeneration of the facet joints. There is no spondylolysis (pars fracture). Also degenerative facets at L6-S1.
The lumbar lordosis has greatly increased. A list of the spine (and possbibly the pelvis) to the left is seen. (no specific mention whether the X-rays were taken erect or not).
MRI REPORT @ SPONDYLOLYSTHESIS CaseFile
Dehydration of the intervertebral discs. (dark colour, a sign of degeneration of the hyaline cartilage).
Anterolysthesis of L5 in relation to L6, Grade 1.
At the L5-L6 level there is canal stenosis due to the forward slip of the vertebra, the degenerative facets and hypertrophy of the ligamentum flavum.
At L6-S1 the canal size is also diminished due to severe facet arthritis and enlargement of the ligamentum flavum. There is possibly a small synovial cyst at the L6-S1 facet joint (left).
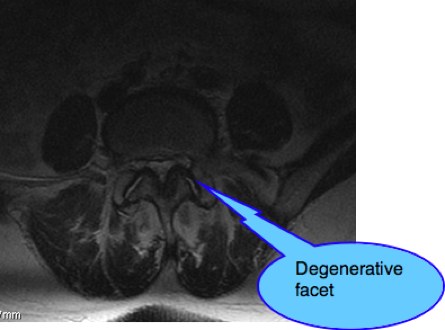
The spinal canal is diminished in size due to the grossly enlarged facets, thickening of the ligamentum flavum (found inside the canal) and, at L5-L6 due to the forward slip of the body of the vertebra L5.
CHIEF COMPLAINT @ SPONDYLOLYSTHESIS CaseFile
A slim 73-year old woman presented with a five year history of pain in the RIGHT buttock radiating to the side of the right thigh and calf.
Two months previously pain in the LEFT low back started, radiating to the back of the left thigh and calf, with tingling on the dorsum of the left foot.
SIGNIFICANT HISTORY @ SPONDYLOLYSTHESIS CaseFile
She was treated by another chiropractor 5 years previously when the pain in the right buttock and leg began, with a 60% improvement over a course of treatment.
Prior, she had had numerous consultations with physiotherapists, a neurologist and her own GP.
Trauma: Five months before the first consultation she slipped on the stairs in her home and fell hard on her sacrum, down four stairs. There was some bruising but no immediate acute low back or leg pain.
Type of pain: A constant nagging ache that she was never during the day without.
Aggravating factors: Turning, setting power with her leg, climbing stairs. Until the recent past she played tennis three days a week.
Relieving factors: Bed rest. She slept well at night.
After a consultation with a neurologist three years previously, the above X-rays and an MRI were taken.
EXAMINATION
The pelvis appeared to be marginally low on the left, suggestive of a left
LEG LENGTH INEQUALITY; a short limb.
A mild left convex scoliosis was evident.
On motion palpation the right sacroiliac joint was fixated. The L4 and L5 joints were tender on palpation, and fixated.
ROM: Lumbar spine flexion and side bending right and left were mildly restricted and painful, with no immediate aggravation of the pain in the legs.
Orthopaedics: Straight leg raising (left leg) provoked mild pain in the left buttock at 60*. Braggards was negative.
The Slump 2 provoked pain in the left buttock and tightness in
the posterior thigh (compared to right) when the left knee was extended. Flip test for sciatica.
Sacroiliac and hip tests were within normal limits.
Neurology: No abnormalities were detected, despite the weak feeling described in the history. Presumed to be a sense induced by pain.
SOAP NOTES @ SPONDYLOLYSTHESIS CaseFile
Consult 1
History and Examination. A simple basic set of exercises were carefully described and demonstrated. To be done on her bed before arising in the morning, and before going to sleep. More often as required.
Consult 2
Report of Findings. Retraced the complex right and left leg pain.
Explanation of the basis of Chiropractic.
Outline of treatment plan:
- 2 consults per week for 4 weeks during which time the pain may increase. Not to be concerned: of a temporary natured, to be controlled with alternating ice and heat packs.
- Rehab phase: 1 treatment per week.
- Gradual reduction of treatment frequency. 1/2w, 1/3w as the condition stabilised.
- A regular treatment 1/6-8 weeks thereafter. A "cure" was most unlikely given the long history of pain and the severe degeneration seen on X-ray.
First treatment:
Adjustment of the pelvis following the Thompson drop protocol on a Lloyd table.
Gentle left-side-down drop on L5. LSD: L6-m.
Active Release Therapy ART of the left piriformis, TFL and hamstring.
Consult 3
S: Right LBP eased, Left LBP worse, no change in left leg pain.
A: Change to RSD adjustment. R: L6-s roll drop, gentle. Supine double knee drop.
Consult 4
S: Increased left LBP. Walking difficult.
O: No change
A: No significant improvement, expected increase in pain.
P: Add gentle roll-drop on L5. R: L6-s, L: L5-m
After treatment still in pain: Return to table: Hard prone drops on the sacrum right and Li Si AS. Supine drops on the ASIS, right and left. Supine pelvic drop.
Consult 5: SPONDYLOLYSTHESIS CaseFile
S: Significantly less pain.
O: Fixation in R sacroiliac joint much improved. Flexion and sidebending and Slump remain painful.
A: More movement, less pain. Progress.
P: Continue treatment as with consult 4. Less vigorous prone drops.
Consult 6
S: Significant improvement. Pain reduced by more than 50%.
O: Slump still painful in the left buttock, less tight in the thigh.
A: Early introduction of gentle rehab exercises as she is going on holiday for three weeks.
P: Add hip-hike, and gentle contraction of neck flexors and extensors with the Pelvic tilt exercise.
- 50 percent less pain is the dangerous time ... √
Consult 7
S: Good holiday, still improving but with some painful days after sitting in the car. Feels she is standing more erect.
O: Flexion much improved, but now increased extension pain.
A: Evaluation of chronic neck pain at next consultation.
P: Treatment as before.
Consult 8: SPONDYLOLYSTHESIS CaseFile
Medical insurance (7 consultations) covers no further treatment. Cancelled next two treatments. Reported continued improvement with exercises.
S: Sudden severe exacerbation of pain, into back of left thigh, and tingling in foot, began three weeks after Consult 7.
O: Increased flexion pain. Slump L unchanged. Worryingly, SLR right reproduces pain in the left leg (crossed sign). SLR left 45* pain in left buttock and left leg. Now a left SI fixation.
A: Possible disc injury L6-S1. On basis of possible medial disc herniation, adjustment with pain side down (lying on left side).
P: L: L6-m gentle drop. Still left Si fixation on motion palpation, so: Prone drops ASAS, left negative Derefield protocol. Three days bed rest, doing exercises every half an hour, ice and heat twice a day, rising at least every hour for a short walk about the house. No sitting or bending whatsoever.
Consult 9 (2d later)
S: 20% less pain.
O: Crossed sign no longer present.
A: Progress
P: Treatment as per consult 7.
Consult 10
S: 50% less pain.
O: Return to pre acute phase. Patient also taking anti inflammatory drugs.
A: Very unstable spondylolysthesis. Introduction of heel lift at next consultation in left shoe.
P: Add gentle roll on L6 left again. Patient to get up for longer periods, some sitting allowed again. However, no housework or car or shopping.
Consult 11
S: No leg pain. Overall 70% improvement in pain and movement.
O: Slump 4 produces no leg pain. A little in the back.
A: Relief! Think doctors don't worry about their patients too?! Two tests confirm that a 5 mm lift reduces her pain, and increases her proprioceptive balance.
P: She may begin to sit again, and is no longer confined to home. I've warned her that the pain diminishes faster than the soft tissues heal. She feels 70% better, but it's probably only 15% healed compared to two weeks ago. We'll see what the next consult in a week brings! One sneeze can change all.
Consult 12: SPONDYLOLYSTHESIS CaseFile
S: No pain in either leg, no back pain. Not taking any medication.
O: Range of Motion of the spine is full and free (though slightly guarded). Slump Test is negative.
A: Hallelujah! The heel lift and the exercises are working.
P: No treatment today. No charge. She's happy obviously, and will return once a week for the following month for control.
This is an extremely unstable back. I've told her she increase
everything by 5% per day. Increasing suddenly by 30% is likely to result
in a relapse. If we can get through the next month with no pain, then
we can breathe a sigh of relief.
DISCUSSION
A degenerative spondy is always going to be tricky. What this lady has in her favour is her excellent weight and general level of fitness. Playing tennis three times a week in her seventies is admirable.
What she has going against her is not only the chronicity of the
case, her short leg and also the extra lumbar vertebra, a so-called
"lumbarisation". This almost always leads to an increased lordosis with
concommitant increased stress on the facet joints. Toning abdominal
muscles will be vital if we are to win with a case like this.
TONING ABDOMINAL MUSCLES ...
This lady is on the verge of major lumbar surgery, for which the
insurance would be paying out 50 000 or more euros, yet they expect the
Chiropractor to win in seven visits. Laughable.
Stopping midway through the programme nearly proved disastrous for her.
She's needed even more treatment than if she came for what was
prescribed, and had a lot of increased pain. The rehab phase is
absolutely vital. She has wisely (I think!) considered the back surgery
alternatives but going through with the full programme is vital in a
case like this.
BACK SURGERY ALTERNATIVES ...
COMPLICATIONS OF SURGERY ...
CHICKEN BONES BOUILLON
This is no misprint. Research at Harvard Medical School found that the gelatine in a chicken bones extract was very effective in managing recalcatrant arthritis. I'll have her start it next week. CHICKEN BONES ...
- Home >
- Lower back pain >
- Spondylolysthesis case file
Did you find this page useful? Then perhaps forward it to a suffering friend. Better still, Tweet or Face Book it.
